Central sleep apnea (CSA) is a disorder in which breathing stops and starts repeatedly during sleep. CSA is caused by a problem with the control of breathing in the part of the brain called the brain stem. Because the brain doesn’t send proper signals to the muscles that control breathing (diaphragm) people with CSA have shallow and slower breathing than normal.
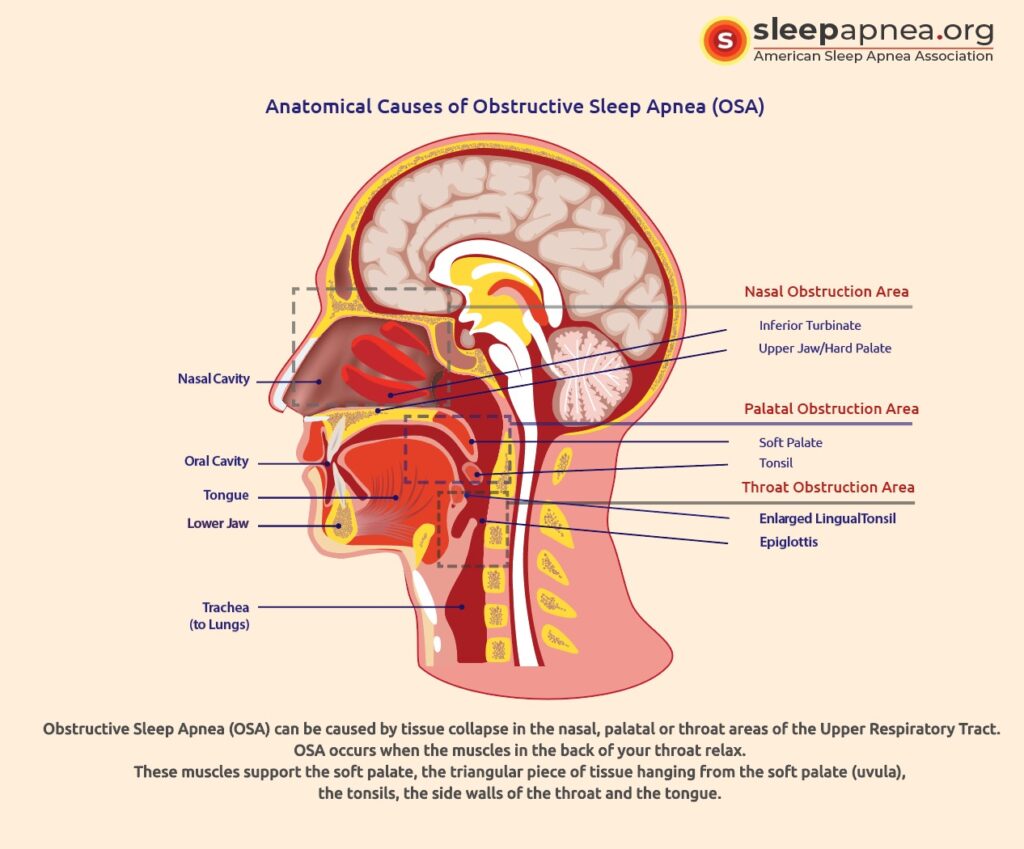
CSA may occur because of other conditions, such as heart failure or stroke. Sleeping at a high altitude (> 6,000 ft) may also cause CSA. Opioids used for pain relief and several other drugs can cause CSA. It is different from Obstructive Sleep Apnea (OSA), a condition in which normal breathing stops because of upper airway obstruction. CSA is much less common than OSA. Unlike obstructive sleep apnea, central sleep apnea is not caused by obesity. While OSA and CSA are separate conditions, they can arise in the same episode of sleep apnea, in what is known as Mixed Sleep Apnea (MSA). Episodes of MSA most often begin as obstructive apneas that are treated.
In addition, treatment of OSA with continuous positive airway pressure (CPAP), can induce treatment-emergent central sleep apnea (TECSA), a form of CSA that manifests after successful treatment of OSA. TECSA is often temporary.
Standard treatments for CSA may involve treating other existing conditions, using a device to assist breathing (CPAP machine) or using supplemental oxygen. Recently the U.S. Food and Drug Administration (FDA) approved an implantable device that stimulates a nerve located in the chest that is responsible for sending signals to the diaphragm to stimulate breathing.
In a healthy patient (without sleep apnea), when carbon dioxide (CO2) levels are high, the brain signals the breathing muscle (diaphragm) to contract at regular intervals, deeper and faster to remove CO2 through exhalation, and vice versa. The signal to breathe travels from the brain stem, down the phrenic nerve, and then to the diaphragm, causing a contraction. This contraction of the diaphragm pulls air into the lungs.
For patients with CSA, the brain stem is less sensitive to changes in CO2 levels, creating a delayed response to sensing levels of CO2 in the blood stream. This delay in CO2 response causes an extended “pause” in breathing, ranging in duration from roughly 10 to 40 seconds. An episode may result in:
- Sleep disturbance
- Decrease in the body’s oxygen levels (also known as hypoxia)
- Surge of nor-epinephrine (the body’s “fight or flight response”, which may feel like a racing heartbeat).
These events can happen multiple times per hour – sometimes as frequently as once per minute. However, these sleep disturbances are often not enough to fully wake the patient. A patient’s sleep partner may be more likely to identify the breathing disorder than the patient himself/herself!
Central sleep apnea (CSA) occurs when your brain fails to transmit signals to your breathing muscles.
CSA can be caused by several conditions that affect the ability of your brainstem — which links your brain to your spinal cord and controls many functions such as heart rate and breathing — to control your breathing.
The cause varies with the type of CSA you have. The 5 main types of CSA are:
- Cheyne-Stokes breathing. This type of CSA is most associated with congestive heart failure, stroke, or kidney failure. Cheyne-Stokes breathing is characterized by a gradual increase and then decrease in breathing effort and airflow, producing alternating rapid breathing (hyperventilation) and shallow breathing (crescendo-decrescendo). During the weakest breathing effort, a total lack of airflow (CSA) can occur.
- Drug-induced apnea. Taking certain medications such as opioids — including morphine, oxycodone, or codeine — may cause breathing to become irregular, or to temporarily stop completely, producing CSA.
- Medical condition-induced central sleep apnea. Several medical conditions, including end-stage kidney disease and stroke, may give rise to a non-Cheyne-Stokes version of CSA.
- High-altitude periodic breathing. A breathing pattern similar to Cheyne-Stokes breathing may occur in people exposed to a very high altitude. The change in oxygen at this altitude causes the alternating rapid breathing and shallow breathing.
- Treatment-emergent central sleep apnea. Treatment-emergent central sleep apnea (TECSA) is a specific form of sleep-disordered breathing, characterized by the emergence or persistence of central apneas during successful treatment for obstructive sleep apnea (OSA). This condition is a combination of obstructive and central sleep apneas, called Mixed Sleep Apnea (MSA). It is often temporary.
- Idiopathic (primary) central sleep apnea. The cause of this uncommon type of CSA is not known. It is essentially a diagnosis of exclusion when all other known causes have been eliminated.
Certain factors put you at increased risk of central sleep apnea (CSA):
- Sex. Males are more likely to develop CSA than are females.
- Age. CSA is more common among older adults, especially adults older than age 65, possibly because they may have other medical conditions or sleep patterns that are more likely to cause central sleep apnea.
- Heart disorders. People with irregular heartbeats (atrial fibrillation) or whose heart muscles do not pump enough blood for the body’s needs (congestive heart failure) are at greater risk of central sleep apnea.
- Stroke, brain tumor or a structural brainstem lesion. These brain conditions can impair the brain’s ability to regulate breathing.
- High altitude. Sleeping at an altitude higher than you are accustomed to may increase your risk of Central sleep apnea (2). High-altitude sleep apnea usually resolves itself a few weeks after returning to a lower altitude. Sleep quality can be improved independent of the presence of CSA by the use of sedation medication.
- Opioid use. Opioid medications may increase the risk of central sleep apnea. May best be treated by alteration or elimination of the drug regimen.
- CPAP. Some people with obstructive sleep apnea develop CSA while using continuous positive airway pressure (CPAP). This condition is known as treatment-emergent central sleep apnea (TECSA). It is a combination of obstructive and central sleep apneas. In most cases TECSA goes away with continued use of a CPAP device. Some people may have to be treated with a different kind of positive airway pressure therapy.
Central sleep apnea is usually asymptomatic and is first detected by caretakers or bed partners. Common signs and symptoms of central sleep apnea include:
- Observed episodes of stopped shallow or abnormal breathing patterns during sleep
- Restless sleep
- Abrupt awakenings accompanied by shortness of breath
- Shortness of breath that’s relieved by sitting up
- Difficulty staying asleep (insomnia)
- Excessive daytime sleepiness (hypersomnia)
- Chest pain at night
- Difficulty concentrating
- Chronic fatigue
- Mood changes
- Morning headaches
- Snoring
- Lower tolerance for exercise
Although snoring indicates some degree of airflow obstruction, snoring also may be heard in the presence of central sleep apnea. However, snoring may not be as prominent with central sleep apnea as it is with obstructive sleep apnea.
If the cause of CSA is a neurological disease, symptoms may also include:
- Difficulty swallowing
- Voice changes, and
- An overall sense of weakness and numbness
Sleep apnea is suspected based on a person’s symptoms. Sometimes doctors use questionnaires during the clinical evaluation to help screen for symptoms, such as excessive daytime sleepiness.
The diagnosis is usually confirmed, and severity is determined in a sleep laboratory by using a test called polysomnography that measures airflow, oxygenation, movement of the abdomen or chest, sound (i.e. snoring), and a variety of other parameters. This evaluation can help doctors distinguish between obstructive and central sleep apnea. However, testing may not be necessary in CSA if there are no symptoms; instead, aggressive management of medical disorders that can cause sleep apnea (eg, heart failure) is tried first.
To diagnose the central nervous system causes of CSA, doctors may ask for brain or brain stem imaging.
reatment options for Central sleep apnea include:
- The primary treatment of central sleep apnea is the treatment of underlying disorders and avoidance of opioids, alcohol, and other sedatives.
- Positive airway pressure (PAP) device. Several types exist, including those that provide continuous pressure (CPAP) and those that provide variable pressure (e.g. BiPAP, ASV). Notably, ASV, or adaptive-servo ventilation, should not be used in patients with chronic, symptomatic heart failure with reduced left ventricular ejection fraction (LVEF ≤ 45%).
- Supplemental Oxygen
- Phrenic nerve stimulation: These devices automatically activate each night to send signals to the breathing muscle (diaphragm) via the phrenic nerve to restore a normal breathing pattern.
- Pharmacologic Therapy: Acetazolamide is effective in central sleep apnea caused by high altitude.
Consult a medical professional if you experience — or if your partner observes — any signs or symptoms of central sleep apnea, particularly the following:
- Shortness of breath that awakens you from sleep
- Intermittent pauses in your breathing during sleep
- Difficulty staying asleep
- Excessive daytime drowsiness, which may cause you to fall asleep while you are working, watching television, or even driving
Ask your doctor about any sleep problem that leaves you chronically fatigued, sleepy, and irritable. Excessive daytime drowsiness may be due to other disorders, such as not allowing yourself time to get enough sleep at night (chronic sleep deprivation), sudden attacks of sleep (narcolepsy) or obstructive sleep apnea.