Table of contents
Obstructive sleep apnea is a potentially serious sleep disorder. It causes breathing to repeatedly stop and start during sleep. Normally adults breathe about 12-16 breaths per minute.
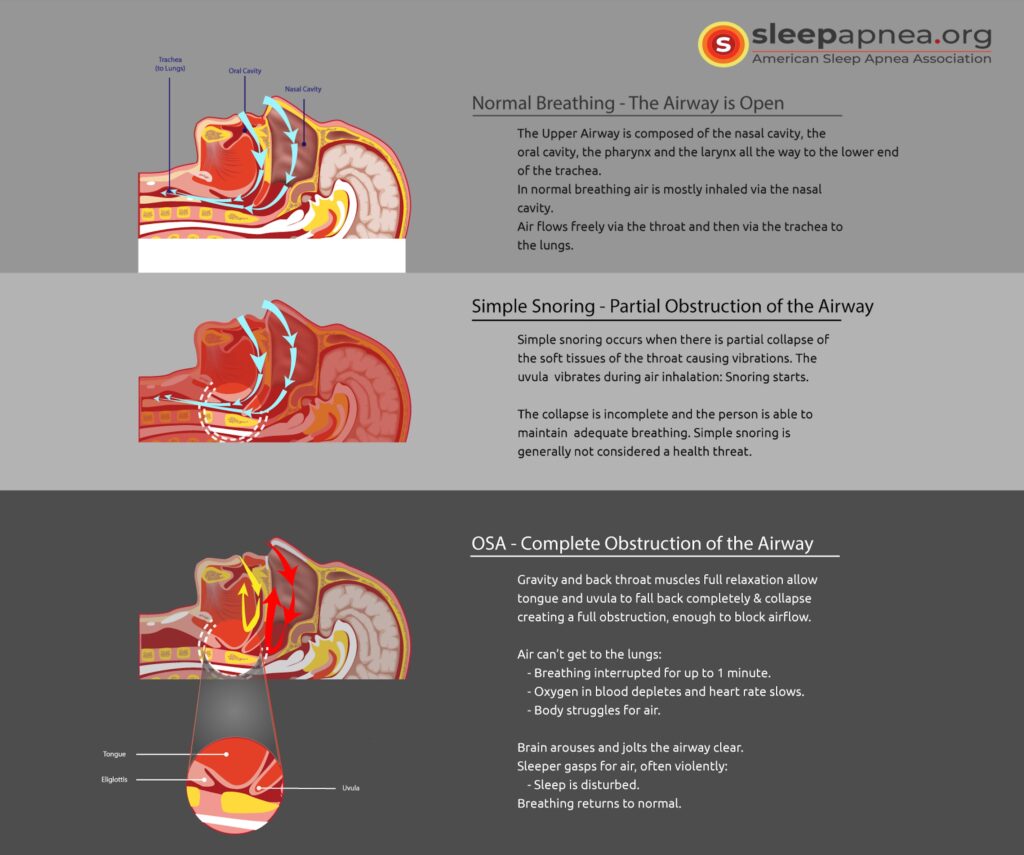
Obstructive Sleep Apnea (OSA) occurs when the muscles relax after you fall asleep. As a result, soft tissue in the back of the throat collapses and blocks the airway. This leads to either a reduction (hypopnea)(1) or pause in breathing (apnea).
There are several types of sleep apnea, but the most common is OSA . This type of apnea occurs when your throat muscles intermittently relax after you fall asleep and block your airway. When you sleep, all the muscles in your body become more relaxed (muscle atonia; paralysis). This includes the muscles that help keep your throat open so air can flow into your lungs. Normally, the throat remains open enough during sleep to let air pass by. Unfortunately, many people have a throat that has narrowed due to one or more causes. When the muscles in the upper throat relax during sleep, that narrow throat closes in and blocks, partially or completely, the airway, leading to either a reduction or a full pause in breathing. This (breathing stopping involuntarily for brief periods of time during sleep) is called OSA .
A noticeable sign of OSA is loud snoring, caused by air squeezing through the narrowed or blocked airway. Many people may not think of snoring as a sign of something potentially serious, and not everyone who snores has OSA , but most people who snore loudly do suffer from OSA. With OSA, snoring usually is loudest when sleeping on your back, and it sometimes quiets when you turn on your side.
If you have been told you snore loudly and regularly it is time to ask your doctor about OSA .
Treatments for OSA are available. The most common treatment involves using a device that uses positive pressure (CPAP, BiPAP, or APAP machine) to keep your airway open while you sleep. Another option is a mouthpiece to thrust your lower jaw forward during sleep. In some cases, surgery may be an option, too.
Learn More About Obstructive Sleep Apnea
Signs and symptoms of Obstructive Sleep Apnea (OSA) you may observe about yourself include:
- Excessive Daytime Sleepiness (EDS)
- Abrupt awakenings accompanied by gasping or choking
- Awakening with a dry mouth or sore throat
- Morning headaches
- Difficulty with concentration or memory, during the day
- Experiencing mood changes, such as depression or irritability
- High blood pressure
- Nighttime sweating
- Decreased libido
Signs and symptoms of OSA your bed partner may observe about yourself, before you are aware of them, include:
- Loud snoring
- Observed episodes of stopped breathing during sleep
- Experiencing mood changes, such as depression or irritability
- Abrupt awakenings accompanied by gasping or choking
Symptoms you both may observe:
- Abrupt awakenings from sleep, often accompanied by choking or gasping
- Decreased libido
- Mood changes or irritability
- Nighttime sweating
- Excessive Daytime Sleepiness (EDS)
- Difficulty with concentration and memory
- Dry mouth or sore throat
- Morning headaches
Risk for OSA increases if you have conditions or features that narrow the upper airway. These OSA risk factors include:
- Children with large tonsils and adenoids
- Men with a collar size of 17 inches or more
- Women with a collar size of 16 inches or more
- Large tongue, which can block the airway
- Retrognathia, which is when your lower jaw is shorter than your upper jaw
- A narrow palate or airway that collapses more easily
You are also at a higher risk for OSA if:
- You are overweight or obese. Although anyone can have sleep apnea, obesity is considered the most important risk factor.
- You have a family history. If obstructive sleep apnea has been diagnosed in other family members, according to the Mayo Clinic, you may be at higher risk.
- You are older. According to the SPELL OUT ALA on FIRST REFERENCE (ALA) obstructive sleep apnea becomes increasingly frequent as you age, leveling off once you reach your 60s and 70s.
- You smoke. OSA is more common in people who smoke.
- You have certain medical chronic conditions such as high blood pressure, diabetes, or asthma.
- You have chronic nasal congestion. OSA occurs twice as often in people with chronic nasal congestion at night.
- You have a crowded pharynx. Anything that makes the pharynx, or upper airway smaller — such as large tonsils or glands — can result in a greater chance for OSA.
A diagnosis of Obstructive Sleep Apnea (OSA) begins with a complete history and physical examination. Your doctor may ask you to fill out a questionnaire about daytime drowsiness, sleep habits, snoring and quality of sleep which can all be important clues. The physical evaluation will examine the back of your throat, mouth and nose for extra tissue or abnormalities. Your doctor may also measure your neck and waist circumference as well as check your blood pressure. You may then get a referral to a sleep specialist for further evaluation to better diagnose your condition, determine the severity of your condition and plan your treatment. That evaluation may involve overnight monitoring of your breathing and other body functions as you sleep (a sleep study), either at-home or in a sleep lab. Finally, your doctor may also refer you to an Ear, Nose and Throat (ENT) doctor to rule out any anatomic blockage in your nose or throat.
Tests to detect obstructive sleep apnea include:
- Polysomnography. During this sleep study, you are hooked up to equipment that monitors your heart, lung, brain activity, breathing patterns, arm and leg movements, and blood oxygen levels while you sleep.
You may have a full-night study, in which you are monitored all night, or a split-night sleep study.
In a split-night sleep study, you will be monitored during the first half of the night. If you are diagnosed with obstructive sleep apnea, staff may wake you and give you continuous positive airway pressure (CPAP) for the second half of the night.
Polysomnography can help your doctor diagnose OSA and adjust positive airway pressure (PAP) therapy, if appropriate.
This sleep study can also help rule out other sleep disorders that can cause excessive daytime sleepiness but require different treatments, such as leg movements during sleep (periodic limb movements) or sudden bouts of sleep during the day (narcolepsy). With REM (rapid eye movement sleep stage) sleep behavior disorder, instead of experiencing the normal temporary paralysis of your arms and legs (atonia) during REM sleep, you physically act out your dreams. The onset can be gradual or sudden, and episodes may occur occasionally or several times a night. The disorder often worsens with time.
- Home sleep apnea testing. Under certain circumstances, your doctor may provide you with an at-home version of polysomnography to diagnose obstructive sleep apnea. This test usually involves measurement of airflow, breathing patterns and blood oxygen levels, and possibly, limb movements and snoring intensity.
The goal for treatment of sleep apnea is to make sure airflow is not obstructed during sleep. Treatment methods include:
Lifestyle Changes and Behavior Modification (2)Those with an obstructive sleep apnea diagnosis will be encouraged to, if necessary:
- Lose weight. Weight loss gives excellent relief from the symptoms of OSA
- Quit smoking
- Participate in regular exercise
- Reduce alcohol consumption
Nasal Decongestants
- Nasal decongestants are more likely to be effective in mild OSA. They can help relieve snoring.
Continuous Positive Airway Pressure (CPAP)
- Nasal CPAP therapy is the first line of treatment for OSA. CPAP is administered through a face mask. The face mask gently delivers positive airflow to keep the airways open at night. The positive airflow props the airways open. The airflow acts as an “invisible” split to keep the airway from being occluded. CPAP is usually a highly effective treatment for sleep apnea. A dental device may also be necessary to keep the lower jaw positioned forward.
Bilevel Positive Airway Pressure (BiPAP or BPAP)
- Bilevel positive airway pressure machines are sometimes used for the treatment of OSA if CPAP therapy is not effective. BiPAP machines have settings, high and low, that respond to your breathing. This means the pressure changes during inhaling versus exhaling.
Positional Therapy
- Since sleeping on the back (supine position) can make sleep apnea worse for some people, positional therapy is used to help those with sleep apnea learn to sleep in other positions. Positional therapy and the use of CPAP can be discussed with a professional at a sleep center.
Oral Appliance
- For patients with mild to moderate obstructive sleep apnea, dental appliances or oral mandibular advancement devices that prevent the tongue from blocking the throat and/or advance the lower jaw forward can be made. These devices help keep the airway open during sleep. A sleep specialist and dentist with expertise in oral appliances for this purpose should jointly determine if this treatment is best for you.
Surgery
- Uvulopalatopharyngoplasty (UPPP, also sometimes called UP3) involves removal of extra tissue from the back of the throat (3). UPPP is the most common type of surgery for OSA, and it helps relieve snoring. However, this surgery has not been proven to eliminate sleep apnea, and it can have complications.
- Tracheostomy may be done as a procedure of last resort. Tracheostomy punctures an opening in the windpipe that bypasses the obstruction in the throat.
- Other surgical procedures may be required to correct structural problems in the face and elsewhere when sleep apnea does not respond to treatments such as CPAP. About 75 percent of children with OSA due to enlarged tonsils or adenoids get relief from surgery. The American Academy of Pediatrics (AAP) has endorsed surgical removal of tonsils and adenoids as the treatment of choice for children with sleep problems due to enlarged tonsils or adenoids.
Obstructive sleep apnea (OSA) can be a severe sleep disorder if your breathing stops and restarts more than 30 times an hour while you sleep. Untreated sleep apnea can have serious long-term effects on your health, such as:
- Heart disease
- Hight blood pressure
- Stroke
- Depression
- Diabetes
There are secondary effects as well, such as automobile accidents caused by falling asleep at the wheel.
According to the Nolo legal network, the Social Security Administration (SSA) does not have a disability listing for sleep apnea. It does, however, have listings for breathing disorders, heart problems, and mental deficits that might be attributed to sleep apnea.
If you do not qualify for the conditions listed, you may still be able to receive benefits through a Residual Functional Capacity (RFC) form. Both your doctor and a claims examiner from Disability Determination Services will fill out an RFC form to determine whether you are able to work due to:
- Your sleep apnea
- The symptoms of your sleep apnea
- The effects of those symptoms on your day-to-day life
Veterans with sleep apnea may qualify for benefits under the U.S. Veterans Administration (VA) Under the VA Ratings Schedule, a veteran with sleep apnea may be entitled to 0%, 30%, 50% or 100% benefits for sleep apnea. Veterans may fill out a questionnaire listed here to submit their claim. https://www.benefits.va.gov/compensation/docs/Sleep_Apnea.pdf
The American Sleep Apnea Association (ASAA) estimates that between 1 and 4 percent of American children have sleep apnea.
Although surgical removal of the tonsils and adenoids is the most common treatment for pediatric obstructive sleep apnea, positive airway pressure (PAP) therapy and oral appliances are also prescribed. For more information on how sleep apnea affects children click here.
References
- Mbata G, Chukwuka J. Obstructive sleep apnea hypopnea syndrome. Ann Med Health Sci Res. 2012;2(1):74-77. doi:10.4103/2141-9248.96943
- Young S. Healthy behavior change in practical settings. Perm J. 2014;18(4):89-92. doi:10.7812/TPP/14-018
- Zhan X, Li L, Wu C, Chitguppi C, Huntley C, Fang F, Wei Y. Effect of uvulopalatopharyngoplasty (UPPP) on atherosclerosis and cardiac functioning in obstructive sleep apnea patients. Acta Otolaryngol. 2019 Sep;139(9):793-797.